Ethics of cure
Our collective health is in danger as many questions and concerns and an uneasy lack of answers rule the medical scenario in the age of quick-fixes.

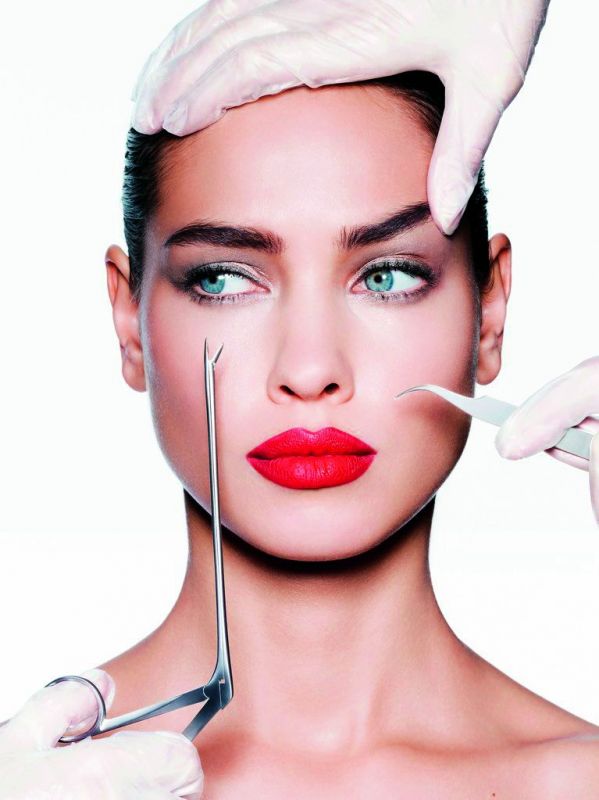
Late actress Sridevi’s sudden demise or that acquaintance you knew who died jogging on a treadmill, or the inexplicable fatality of someone relatively healthy... those concerns are on everyone’s minds. Was it weight loss pills, or exercising too much or quick fixes or lack of proper knowledge that played a part? Were they advised about the serious side-effects? With the incidence of heart attacks, needless C-sections, and lack of proper communication between doctor and patient, health sits in uneasy silence. Diagnosis through websites, needless interventions and surgeries, and corporate medicine. Is it time to take a step back on how we embrace medicine and find answers to questions that are plaguing us?
The scenario
India is considered the C-section capital of the world and is among the highest in diabetics, hypertension and cardiac problems. Medicine has become an industry, a corporate juggernaut where clarity in terms of a patient getting information, and accountability on the doctor’s side, both have suffered. Bariatric surgery is the rage but has many side-effects, fertility treatments are the go-to and can cause clots and strokes, even cholesterol tablets have side-effects that many are not aware of. Heart health is worrying. Are ordinary individuals aware of these quick fixes and adverse effects? Or does corporate medicine rule? For instance, when Sumita Vedeyi, 35, and her husband decided to go the IVF way, they were coached on what happens, what to expect and the process. Yet, one thing they did not know were the effects of the pills, injections and how hormonal treatment can play havoc on health. A specialist (who prefers to remain anonymous), explains, “A doctor will explain a procedure, effects. But some don’t delve into the negative effects — that is their way. If one is taking injections, pills etc, the onus of reading about it is on the patient. In a perfect world, the pharmacist guides you, but not in India! The patient has to come to their own conclusion.”
But what of the quick remedies today’s patients want? Dr Karunesh Kumar HS, senior consultant, Internal Medicine, Columbia Asia Hospital, Sarjapur Road cautions, “A quick fix can never be a solution to weight loss. Diet pills/fad diets all will ultimately lead to increased weight as the physiological secretion of hunger hormone ghrelin increases after extreme dieting, and a person may actually put on more weight. Diet without supervision can lead to liver, kidney and digestion problems. Kidney function and liver function tests should be done when on a ketogenic diet. Electrolyte imbalances like disturbances in sodium and potassium levels can happen with quick fixes. Slow and steady wins.”
 C section rates in our country are very high.
C section rates in our country are very high.
Can you stomach it?
Bariatric surgery, a rage, is only applicable to obese patients but many are resorting to it for weight loss. Dr C.A. Prashanth, consultant, gastrointestinal and laparoscopic surgeon, Fortis Hospitals advises, “Bariatric surgery is known as metabolic surgery, and is the in-thing for obese patients. The main criteria presently is those with a BMI > 40 or BMI > 35. The patient undergoes multidisciplinary evaluations, physician/endocrinology, blood tests, psychiatrist evaluations to identify the cause for obesity. If any hormonal ailments are detected, he or she is then treated to avoid surgery. We also do an endoscopic evaluation to rule out any H Pylori infections that needs attention before surgery.” But Dr Prashanth cautions, “The main or uncommon complication of any bariatric surgeries are leaks —if the surgeon is experienced and trained in laparoscopic stapling and suturing techniques, these complications are avoided!”
As for weight loss pills, according to webMD,com, there are fat trappers like chitosins that prevent fat from being digested, and fat burners that can cause fatal heart attacks, aarhythmias and strokes. Most doctors and dieticians prescribe exercising, cutting down on portion sizes to increase metabolism. A recent incident of a man in Chennai who took slimming drugs from an online quack shows the trend among many to opt for such pills. Dr Karunesh Kumar, senior consultant, Internal Medicine, Columbia Asia Hospital busts some beliefs, “Only five drugs are approved by FDA for weight loss. Orlistat prevents absorption of fat in the intestine so that excess fat is excreted in stools. If a meal is rich in fat, this drug is useful. In a carbohydrate-rich meal (Indian diet) it is of no use. It causes dyspepsia, loose stools and abdominal discomfort in few cases. Ilraglutide (saxenda) is an injection taken daily, which is a medicine for diabetes mellitus. It causes satiety (feeling of fullness), delays gastric emptying but causes nausea and abdominal discomfort. It costs around Rs 10,000 a month. Topiramate is used for epilepsy and migraines. The other quick fixes are diets like Atkin’s, GM, keto.”
Dr Prashanth also advises patients to be prudent, “Orlistat’s efficacy is not proven. Side-effects are calcium and vitamin disorders and gastrointestinal disorders.” But the fad of instant gratification is a part of this smartphone generation. Nutritionist Aruna Vijay agrees, “People today don’t go traditional in diet, health and exercise. They tend to follow new fads. Following diets blindly gives temporary benefits. All these diets are yo-yo and in the long run, prove harmful. Slimming pills give temporary benefits and adequate research too has not been done,” she says. Patients, too, come in for quick solutions. What can a doctor do? “Patients should be wary of any non-professionals, giving treatment for weight loss without any scientific evidence! One should follow a strict diet which is calorie based and a well-modulated exercise pattern guided by professional trainers,” says Dr Prashanth.
The surgical conundrum
The American Medical Association called for a congressional hearing on unnecessary surgery, claiming that there were “2.4 million unnecessary operations performed on Americans.” In India, the numbers are quadrupled or more. Arthroscopic partial meniscectomy, one of the most commonly performed surgical procedures in the world, allows treating internal knee damage through small percutaneous skin incisions. In the United States alone, approximately 700,000 arthroscopic partial meniscectomies are done every year. Consider this provocative analogy — if surgery were a pharmaceutical drug, the procedure would be required to undergo scrutiny of testing and trials and approval by the Food and Drug Administration. Yet, we do not regulate surgical procedures.
The See Section
The World Health Organisation has long recommended that the ideal c-section rate should be between 10-15 percent. When c-section rates in a country move towards 10 percent, there is a significant decrease in maternal and newborn deaths. In another report by an international news agency, the latest (2017) Indian government data show rates in some Indian states are much higher. The rate of C-section deliveries in private hospitals tops 70 percent in West Bengal and is almost 75 percent in Telangana. Even Australia with its well-oiled health system, reports of high c-sections at private hospitals. So where does that leave our country?
Payal Shah and her husband planned a natural delivery when their gynaecologist preponed a C-section due to other commitments. Dr Gayathri D Kamath, consultant, obstetrics and gynaecology, Fortis Hospitals explains traditional medical wisdom, “It is essential that we as obstetricians encourage women to have natural birth. The benefits outweigh the risks of Caesarean section. Women who deliver normally recover faster, and are faster in their subsequent pregnancies, are likely to resume activities earlier. However be apprised of certain unpredictable elements. Fortunately, these happen rarely and most women deliver healthy babies.” Dr Gayatri cautions on adverse effects too, “Caesarean sections are performed only when there are medical conditions justifying it. Some women demand a planned Caesarean section. As health care providers, it is essential for us to spend some time with such women. If they opt for a c-section fearing pains, we offer pain relieving options — epidural or inhalation of nitrous oxide that are considered safe.”
While serious risks of a c-section are rare, in adverse cases, wound infections and scars can take long to heal and bleeding can occur. Pregnant women with blood that clots easily, surgeries, immobility, obesity and smoking enhance the tendency of blood clots. The other aspect of pregnancy is the rage for after-pregnancy weight loss. Dr Gayatri recommends, “Myths and deep rooted beliefs make women overeat ghee and high calorie foodstuffs which make them obese. Women should resume day to day activities gradually, and have a well-balanced diet. Any women can get back to regular workouts in six weeks, irrespective of the mode of delivery.”
Yet, what if a client insists? Dr Gayatri advises, “Women who demand it for no reason should be counselled on the pros and cons and their fears and concerns should be addressed.” With many instances of epidurals gone wrong, she advises that benefits and drawbacks of epidurals should be discussed with the anaesthetist in the antenatal period. When it comes to infertility treatment too, there is an increased incidence of miscarriage, hot flashes, nausea and breast tenderness. It can also cause ovarian cysts and pelvic discomfort from over-stimulation of the ovaries. But many are unaware of these effects. Reactions and course of action also differ from patient to patient, as there is no one rule for all.
Money matters
Today, getting admission in a medical college, in popular specialities like surgery, radiology, etc has a capitation fee of around '1 crore which many ordinary individuals cannot think of repaying even in one lifetime. Then there is health care for profit. “Many larger hospitals run as a corporate structure. And each doctor gets a cut from the tests ordered, be it an MRI or Pet Scan or even blood tests, which will obviously lead to more testing, even if not required. Infact, those that do not like to prescribe to surgeries and prefer non-interventionist solutions are outcast, patients are not sent to them. Take for instance a doctor who touts a 99 percent success rate, and another doctor who says, 75 percent, and also details side effects. Which one will you choose? Obviously the 99 success rate. Some patients are not satisfied unless there is a major intervention too. So, who do you blame?” says the specialist.
The traditional GP
Corporate medicine today is guided by drastic targets. If you add patients without patience, the medical scenario in India is one of trepidation, and worrying. But to understand this dilemma, we need to go back to olden day medicine. “Gone are the neighbourhood GPs, and instead large corporates run hospitals and patients demand specialists,” explains the specialist. We should have a system where the first point of contact for someone ill, is the neighbourhood GP, who checks and prescribes care for minor issues. Only in complications, do they refer a specialist. In India, patients skip this process, and go to a specialist for a chest pain which could be indigestion. Predictably, a cardiac specialist orders a bevy of needless tests, to rule out any issues.” So who is to blame? The medical board who “is busy deepening pockets starting medical colleges,” adds the specialist, and “targets” of course.
Needless surgeries
The specialist surgeon delves deeper, “Hospitals are pushing doctors. If you don’t operate on enough patients, they will not send you patients, who will be sent to doctors who do surgeries. Today’s medical scenario is commercialised. There are reports that say doctors get cuts — 40 per cent for MRIs and 30 to 40 per cent for blood tests, even. Unwanted surgeries are rampant. But what is most frightening is that doing unwanted tests might cost one more money, but doing unwanted surgeries can put your life at risk.”
Holistic courses, not specialised ones
“Some doctors give unrealistic expectations and when the outcome is not desirable, there are many instances of patients beating up doctors,” he says, adding, “Getting expert opinions, and treading the path of caution is best. There is a dire need to change the way we do and perceive medical intervention. We have patients who want quick solutions, and think the more money they pay, the better they will be cared for. They feel the need to see only specialists. And doctors guided by targets and cuts in huge corporate hospitals. Sadly, our MBBS courses today are not designed for holistic medicine, but specialisation too.” Unless we go back to our teaching methods, and formulate guidelines, our collective health is in danger.
